What Is the Endometrium? Structure, Function & Health Explained
Introduction — Why Understanding the Endometrium Matters
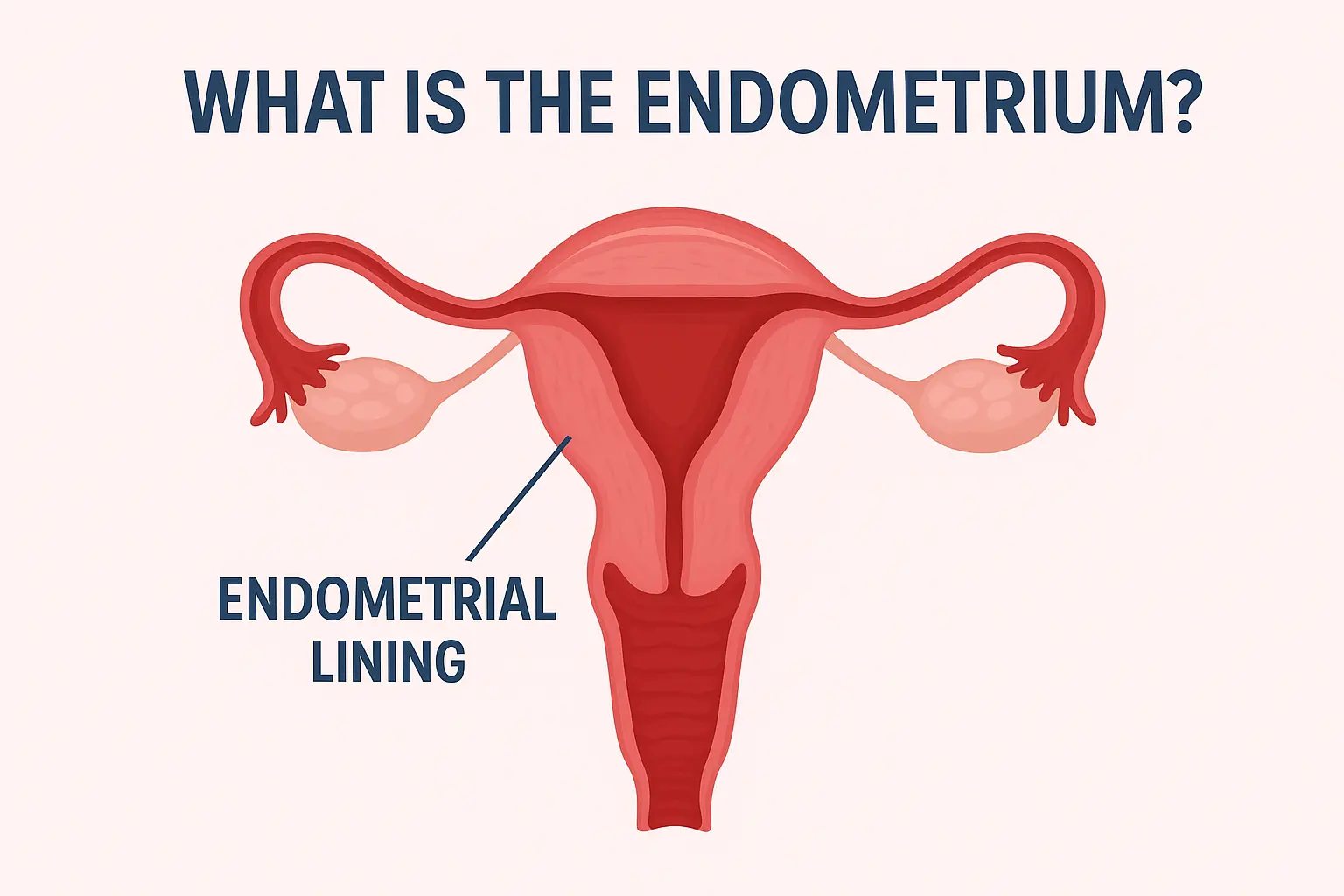
The inner lining of the uterus, known as the endometrium, is far more than simply the “uterine lining”. It is a dynamic, hormone-responsive tissue that undergoes monthly cycles of growth, preparation for pregnancy, shedding, and regeneration. This lining is the tissue that is shed during menstruation and also the very site where an embryo implants if pregnancy occurs.
Understanding the endometrium matters for reproductive health, menstrual disorders, fertility, and for recognizing when things are not functioning normally. In this article we explore what the endometrium is, how it works, what can go wrong, and how to maintain its health.
Anatomy of the Endometrium
The uterus is made up of three primary layers: the outermost serosa (perimetrium), the thick muscular layer (myometrium), and the innermost mucosal lining, the endometrium.
Layers of the Endometrium
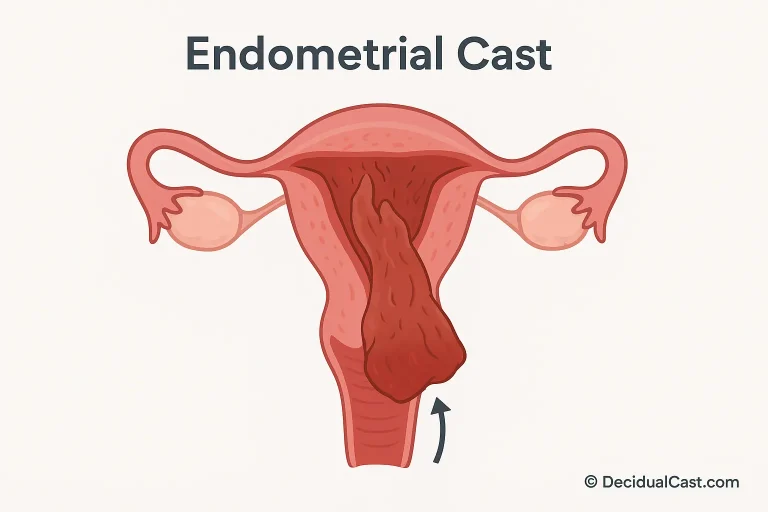
The endometrium itself is divided functionally into two layers: the basal layer (stratum basalis) and the functional layer (stratum functionalis).
- Stratum basalis – this is the deeper layer adjacent to the myometrium; it remains relatively stable and serves as the source of regeneration.
- Stratum functionalis – this is the layer that thickens during the menstrual cycle under hormonal influence, and if no implantation occurs, is shed during menstruation.
Microscopically, the endometrium consists of epithelial cells lining the uterine cavity, tubular glands extending into the stroma, a connective stroma with immune and vascular cells, and abundant blood vessels, notably the spiral arteries.
How the Endometrium Changes During the Menstrual Cycle
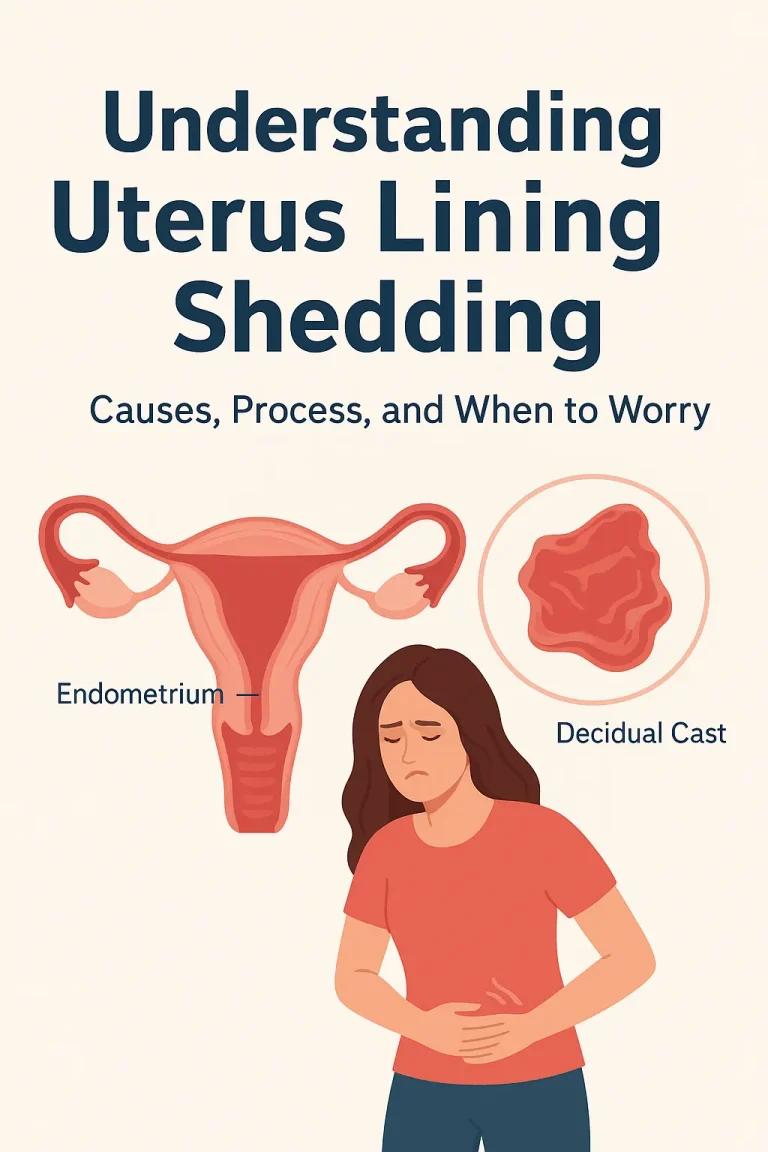
The endometrium is not static. Driven by ovarian hormones (primarily estrogen and progesterone), it undergoes cyclical changes to prepare for possible pregnancy and, if that does not occur, is shed.
Proliferative Phase (Follicular Phase)
After menstruation, rising estrogen levels stimulate the functional layer to rebuild and thicken. Glands elongate, stroma becomes vascularised, preparing for a potential fertilised egg.
Secretory Phase (Luteal Phase)
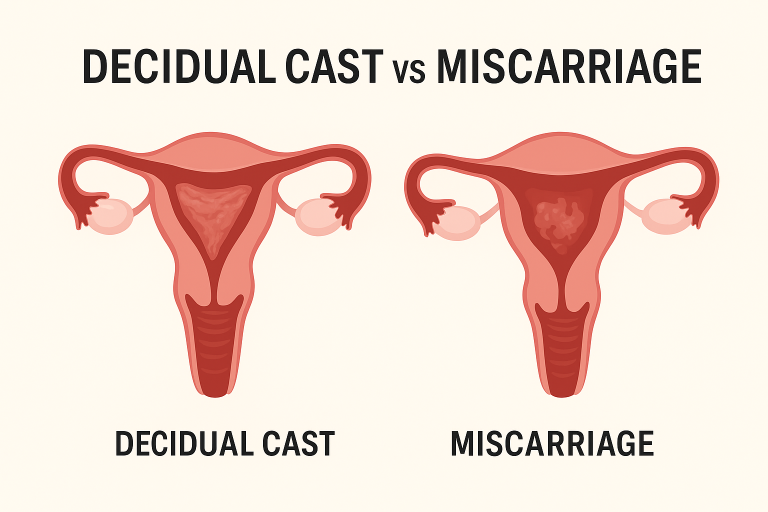
Following ovulation, progesterone from the corpus luteum triggers the stroma to decidualize (in pregnancy) or to change into a receptive lining. The glands begin secretion of nutrients. If implantation occurs, the endometrium becomes the maternal part of the placenta. If not, this phase will lead into shedding.
Menstrual Phase
If fertilisation does not occur, the drop in progesterone causes the spiral arteries to constrict, the functional layer becomes ischemic, and then sheds as menstruation. The basal layer remains intact to regenerate the lining for the next cycle.
In essence, the endometrium cycles through build-up → secretory adaptation → breakdown, typically every 28 days in reproductively active individuals.
The Endometrium’s Role in Fertility and Pregnancy
The endometrium is central to reproduction. It provides the site for implantation of the embryo and supports early pregnancy. Without a properly prepared endometrium, implantation may fail.
Endometrial Receptivity and Decidualization
Once a fertilised egg (blastocyst) arrives, it must implant in a receptive endometrium. The stroma undergoes decidualization—transformation of stromal cells into secretory decidual cells—to allow proper interaction with the embryo.
Implications for IVF and Fertility Treatments
In fertility‐medicine, the thickness, pattern and receptivity of the endometrium are key metrics. Abnormal endometrial lining (too thin or disrupted) can contribute to implantation failure or recurrent miscarriage.
Common Endometrial Conditions and Disorders
Although the endometrium typically functions smoothly, several disorders may affect its structure and function. Early detection and management matter.
Endometritis (Infection/Inflammation)
Endometritis is inflammation of the endometrium often following childbirth, miscarriage, or instrumentation (e.g., IUD insertion). Symptoms can include pelvic pain, fever, abnormal bleeding; treatment is antibiotics and follow-up.
Endometriosis
Though technically outside the uterine lining, “endometriosis” involves tissue similar to the endometrium growing outside the uterus (ovaries, pelvic cavity) and can cause pain, heavy periods, and infertility.
Endometrial Hyperplasia & Endometrial Cancer
Endometrial hyperplasia refers to abnormal thickening of the lining (often from excess estrogen without progesterone). If atypical cells develop, the risk of progressing to endometrial cancer rises.
Other Disorders (Thin Endometrium, Asherman’s Syndrome)
A thin endometrium, scarring (intra-uterine adhesions, “Asherman’s syndrome”), or irregular cyclic build-up can impair fertility or cause abnormal bleeding.
How Doctors Examine the Endometrium
Evaluation of the endometrium typically involves non-invasive imaging and/or direct sampling, depending on the clinical scenario.
- Transvaginal ultrasound: measures endometrial thickness and pattern. Normal ranges vary across the cycle and after menopause.
- Endometrial biopsy / sampling: to assess for hyperplasia, cancer, infection, or determine endometrial receptivity in fertility settings.
- Hysteroscopy: direct visualization of the uterine cavity may be used for structural assessment (polyps, adhesions).
Proper evaluation enables diagnosis of underlying problems such as abnormal uterine bleeding, infertility, or chronic pelvic pain.
How to Keep Your Endometrium Healthy
Healthy endometrial function is supported by both lifestyle and medical management when needed.
- Balance your hormones: Maintain a healthy weight, manage stress, and sleep well — all influence estrogen and progesterone levels.
- Treat infections promptly: Ensure any pelvic or uterine infections are diagnosed and managed to avoid damage to the lining.
- Regular gynecological check-ups: Especially if you have abnormal bleeding, infertility, or are using hormonal therapies.
- Healthy lifestyle: Exercise moderately, avoid smoking, consume a balanced diet rich in antioxidants — all support uterine health.
Regeneration & Endometrial Stem/Progenitor Cells
A remarkable feature of the endometrium is its ability to regenerate roughly 400-500 times over a reproductive lifespan. This is made possible by a population of endometrial stem/progenitor cells located in the basal layer.
These stem cells enable rapid tissue repair after shedding (menstruation) and enable the cyclical nature of the endometrium. Abnormalities in these stem cells are being investigated in relation to infertility, endometriosis, and endometrial cancer.
FAQs — Frequently Asked Questions
What does a healthy endometrium look like on ultrasound?
During the menstrual phase, the lining may measure 1–4 mm; during proliferative phase, ~5–11 mm; and in the secretory phase up to ~14–18 mm in reproductive-age individuals. After menopause, less than ~5 mm is typical.
Can the endometrium heal after being damaged?
Yes. Provided the basal layer is intact, the endometrium regenerates each cycle. However, damage to the basal layer (e.g., by repeated surgery or infection) may lead to scarring and reduced function.
Does endometrial thickness affect fertility?
Yes — insufficient thickness, poor pattern, or receptivity issues (timing, hormonal support) can contribute to implantation failure. Clinics often monitor this in IVF or recurrent miscarriage cases.
When should I talk to a doctor about menstrual/uterine lining issues?
If you experience heavy or prolonged bleeding, bleeding after menopause, irregular cycles, or fertility issues — a gynecologic evaluation is recommended. These may indicate underlying endometrial disorders.
Key Takeaways
- The endometrium is the innermost lining of the uterus, and is central to menstruation, fertility and pregnancy.
- It consists of a stable basal layer and a cyclical functional layer that builds, supports pregnancy if needed, then sheds if no pregnancy occurs.
- Proper hormonal regulation (estrogen/progesterone) is essential to healthy endometrial function and receptivity.
- Many conditions (infection, hyperplasia, scarring, abnormal thickness) may affect the endometrium and require clinical evaluation.
- Lifestyle factors, timely medical care, and fertility-awareness contribute to maintaining healthy endometrial lining and reproductive outcomes.