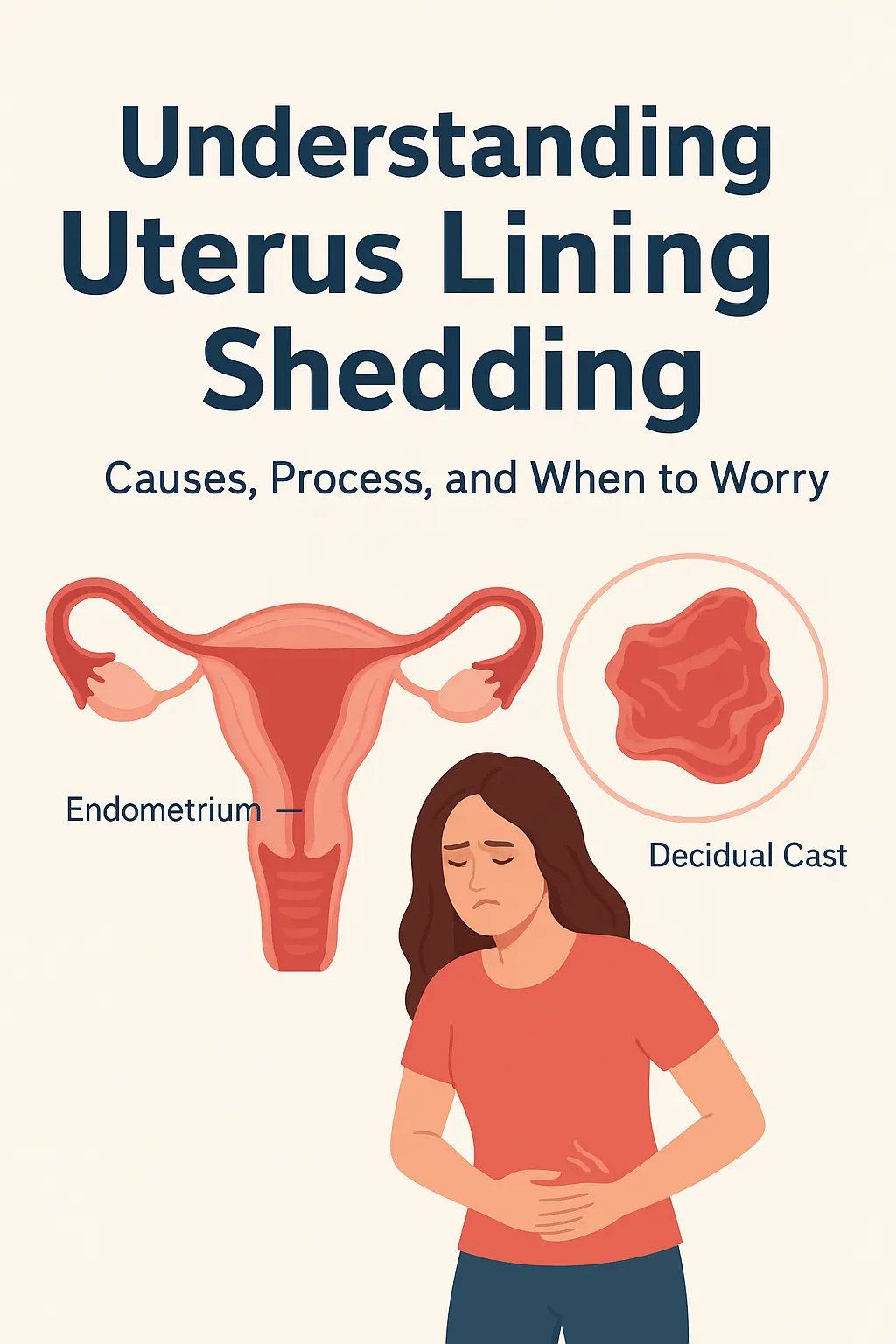
Understanding Uterus Lining Shedding: Causes, Process, and When to Worry
Introduction
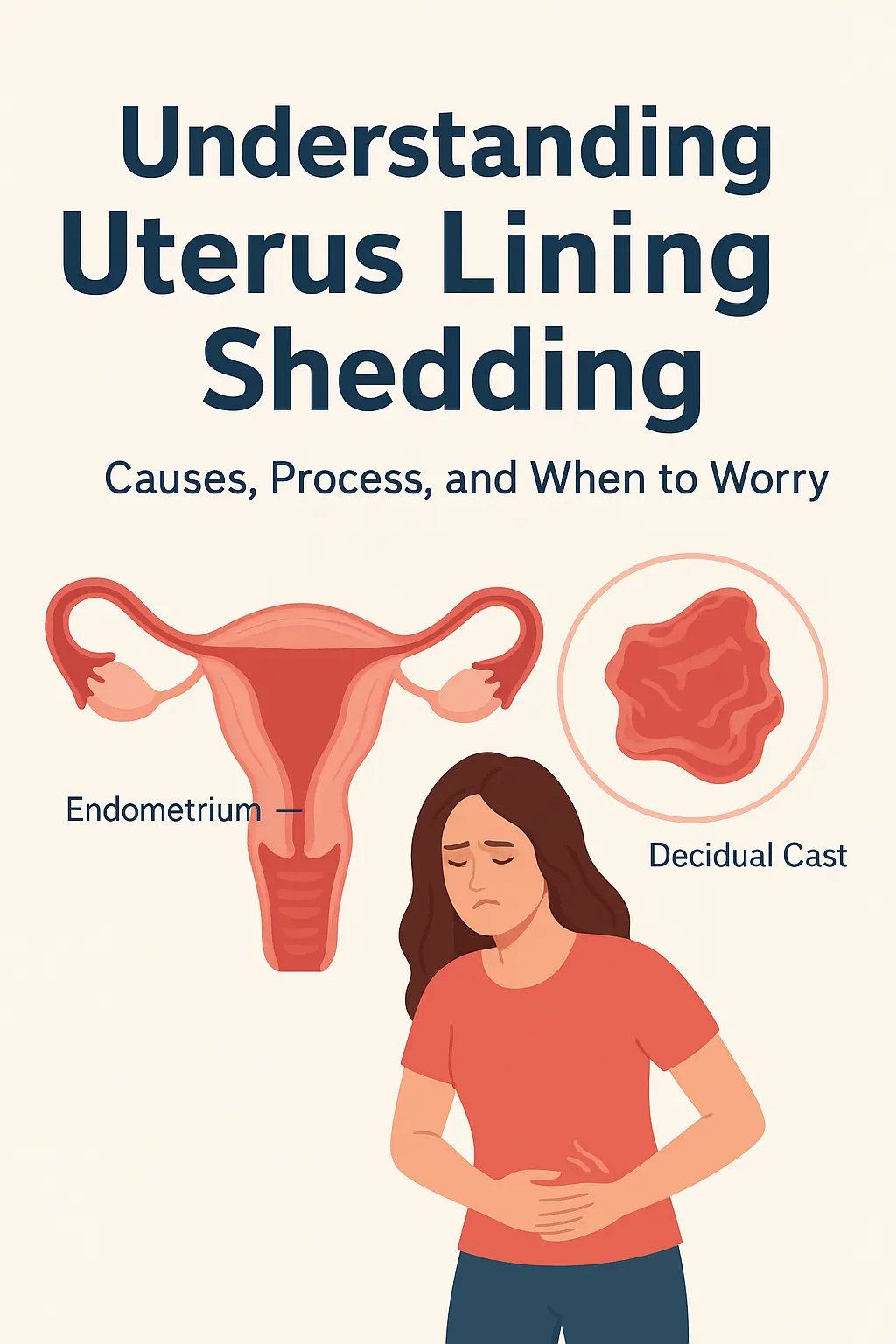
Every month, the female body prepares for a potential pregnancy. The uterus builds a soft, nutrient-rich layer called the endometrium, or uterine lining. When pregnancy doesn’t occur, this lining breaks down and is shed — resulting in menstruation.
Shedding of the uterine lining is a natural and essential process of the menstrual cycle. However, sometimes this shedding may appear unusually heavy, painful, or even occur in one large piece, such as in the case of a decidual cast.
In this article, you’ll learn how the uterine lining sheds, what’s normal versus abnormal, possible causes of heavy or irregular shedding, and when to seek medical attention.
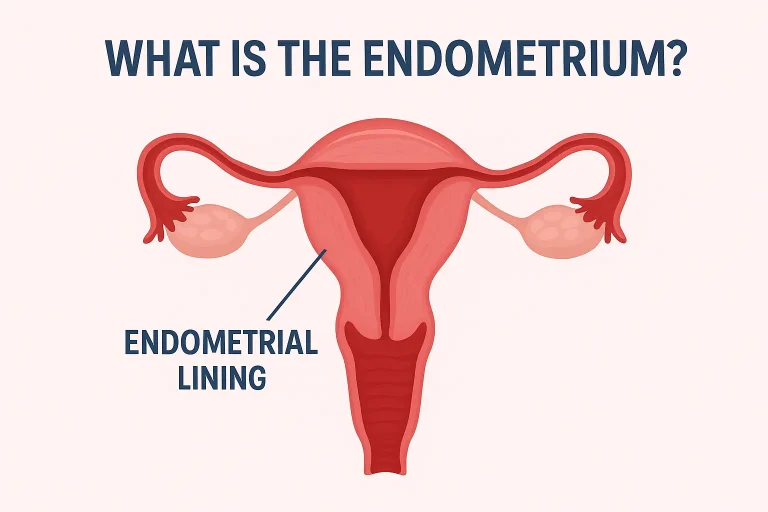
What Is the Uterine Lining?
The uterus is a hollow, pear-shaped organ that houses and nourishes a fertilized egg during pregnancy. Its inner layer — the endometrium — plays a central role in reproduction.
The endometrium consists of two layers:
- Stratum functionalis (functional layer): builds up under hormonal influence and sheds during menstruation.
- Stratum basalis (basal layer): remains intact after menstruation and regenerates the functionalis for the next cycle.
In short: the uterus lining renews itself every month to prepare for pregnancy, and if no pregnancy occurs, the outer layer breaks away as menstrual blood.
How the Uterine Lining Builds and Sheds (Menstrual Cycle Phases)
The menstrual cycle is governed by changes in estrogen and progesterone levels. It has three major phases:
1. Proliferative Phase (Days 5–14)
- Controlled mainly by estrogen.
- The endometrium thickens and blood vessels multiply.
- The uterus prepares to receive a fertilized egg.
2. Secretory Phase (Days 15–28)
- After ovulation, progesterone from the corpus luteum stabilizes the thickened lining.
- Glands secrete nutrients for a potential embryo.
3. Menstrual Phase (Days 1–5)
- If fertilization doesn’t occur, hormone levels fall.
- Blood supply to the endometrium is cut off, tissue breaks down, and the uterine lining sheds.
- This breakdown results in menstrual bleeding.
Fun fact: The endometrium is one of the few tissues in the body that regenerates regularly throughout a woman’s reproductive life.
Normal Uterine Lining Shedding (Menstrual Period)

Menstruation is the visible part of the uterine shedding process.
A typical period involves:
- Cycle length: 21–35 days.
- Bleeding duration: 3–7 days.
- Blood loss: usually less than 80 mL.
The menstrual flow consists of blood, mucus, and small fragments of endometrial tissue. You may notice tiny clots or stringy material — this is normal.
What normal shedding looks like:
- Color: bright red to dark maroon.
- Texture: smooth with occasional soft clots.
- Pain: mild to moderate cramps, manageable with rest or NSAIDs.
What Causes Abnormal or Excessive Shedding?
Sometimes the uterine lining doesn’t shed normally. You may notice heavy bleeding, irregular cycles, or clots larger than a coin.
Doctors classify such problems under Abnormal Uterine Bleeding (AUB), explained using the FIGO PALM–COEIN system:
Structural Causes (PALM)
- P — Polyps: Small tissue growths inside the uterus that cause spotting or heavy bleeding.
- A — Adenomyosis: Endometrial tissue grows into the uterine wall, causing pain and heavy flow.
- L — Leiomyoma (Fibroids): Benign muscle tumors that can distort the uterus and increase bleeding.
- M — Malignancy/Hyperplasia: Uncontrolled cell growth, sometimes precancerous.
Functional or Non-Structural Causes (COEIN)
- C — Coagulopathy: Blood clotting disorders (like von Willebrand disease) that cause excessive bleeding.
- O — Ovulatory Dysfunction: Irregular ovulation from PCOS, stress, or thyroid disorders.
- E — Endometrial Causes: Local infection or inflammation.
- I — Iatrogenic: Caused by medications (e.g., birth control pills, anticoagulants).
- N — Not Otherwise Classified: Rare or unexplained conditions.
Note: Chronic stress, rapid weight changes, and hormonal imbalance can also affect the uterine lining’s stability and lead to erratic shedding.
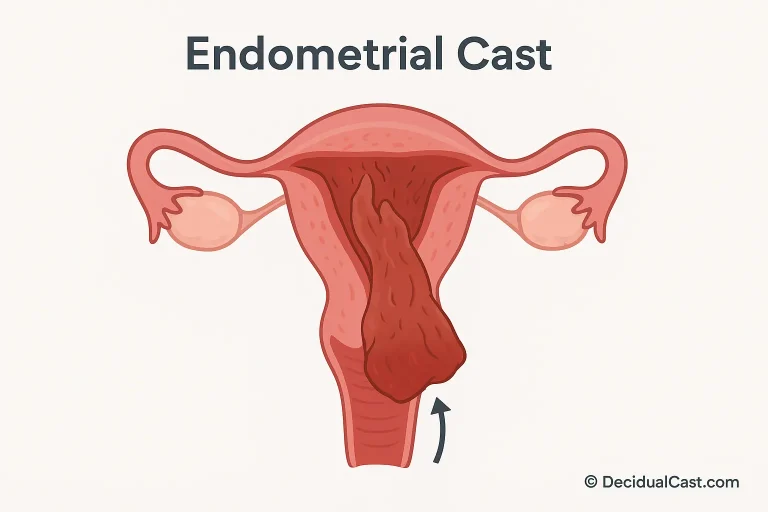
Decidual Cast — When the Entire Lining Sheds at Once
One of the most striking (and alarming) uterine shedding events is called a decidual cast.
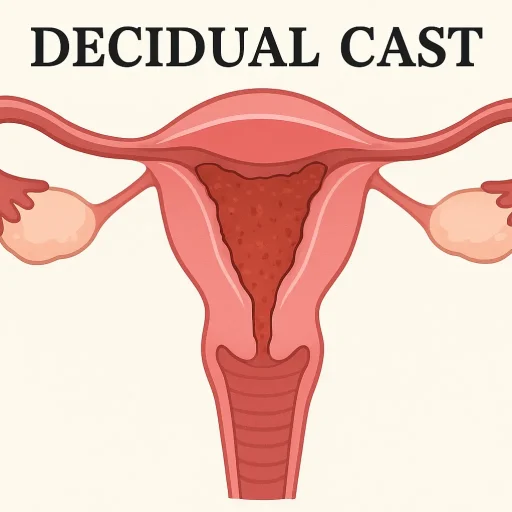
What it is:
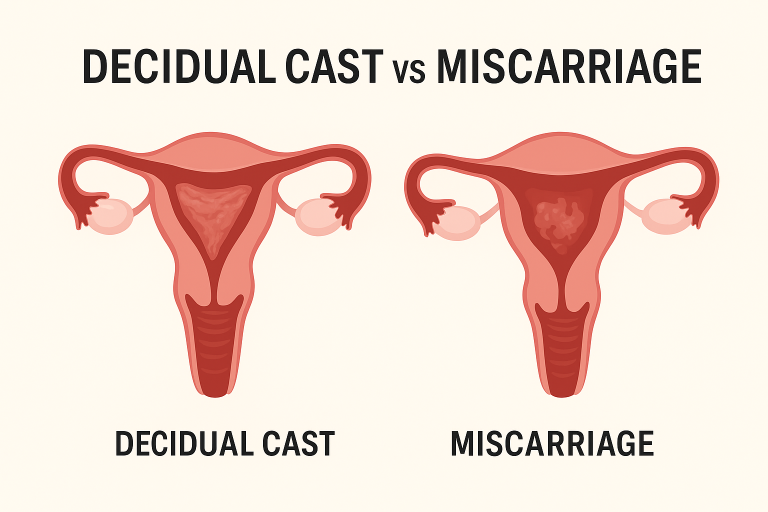
A decidual cast occurs when the entire endometrial lining is expelled in one large piece, often shaped like the inside of the uterus. It’s rare but can cause intense cramps followed by the passage of tissue that looks like a “uterine mold.”
Common symptoms:
- Sudden, severe cramping or sharp pelvic pain.
- Passing a large piece of tissue, sometimes with a triangular shape.
- Temporary relief after the tissue is expelled.
Possible causes:
- Hormonal fluctuations (especially progesterone surges or withdrawal).
- Early miscarriage or ectopic pregnancy.
- Use or discontinuation of hormonal birth control.
- Stress or infection affecting uterine contractility.
Treatment:
Usually conservative. Doctors may recommend rest, hydration, and pain management.
A pregnancy test and ultrasound are essential to rule out miscarriage or ectopic pregnancy.
Important: If you pass a large piece of tissue, save it for medical examination — it helps identify whether it’s a decidual cast, miscarriage tissue, or other pathology.
Symptoms That Indicate Abnormal Uterine Shedding
Call your healthcare provider if you experience:
- Heavy bleeding soaking through pads/tampons every hour.
- Periods lasting longer than 7 days.
- Passing large clots or tissue fragments.
- Severe pelvic pain, dizziness, or fainting.
- Bleeding between periods or after intercourse.
- Post-menopausal bleeding.
Tracking your symptoms and cycle duration in a period app can help your doctor identify patterns and underlying causes.
Diagnosis: How Doctors Evaluate Uterine Lining Issues
A doctor will assess uterine shedding issues through multiple steps:
1. Medical History & Physical Exam
- Period patterns, pain level, medications, and sexual activity.
- Family history of bleeding disorders.
2. Laboratory Tests
- Pregnancy test (β-hCG): to rule out pregnancy or miscarriage.
- Blood count (CBC): to detect anemia.
- Hormone panel: for thyroid, prolactin, estrogen, and progesterone.
- Coagulation profile: if bleeding disorder suspected.
3. Imaging
- Transvaginal Ultrasound: first-line imaging to view endometrial thickness and detect fibroids or polyps.
- Hysteroscopy: a small camera inserted through the cervix to inspect the uterus directly.
- MRI: for detailed mapping in complex cases like adenomyosis.
4. Biopsy
If needed, a small endometrial sample is taken to check for infection, hyperplasia, or cancerous changes.
9. Treatment Options
Treatment depends on the cause, severity, and whether you want to preserve fertility.
Medical Management
- NSAIDs (e.g., ibuprofen): reduce prostaglandins and blood flow.
- Tranexamic acid: helps blood clot and reduces bleeding.
- Hormonal therapy: birth control pills, progestins, or IUDs to regulate hormones and cycles.
Surgical Procedures
- Polypectomy or Myomectomy: removal of polyps or fibroids.
- Endometrial Ablation: destroys the uterine lining to reduce heavy bleeding.
- Hysterectomy: complete uterus removal (last resort).
For Decidual Casts
- Symptomatic treatment: rest, hydration, pain relief.
- Ensure no underlying infection or pregnancy-related issue.
10. When to Seek Medical Help
Immediate medical attention is necessary if:
- You soak through pads hourly for several hours.
- You feel dizzy, weak, or faint.
- You have fever, chills, or foul-smelling discharge.
- You pass large intact tissue or suspect a pregnancy loss.
- You have post-menopausal bleeding.
Early diagnosis ensures effective treatment and prevents serious complications like anemia or infection.
11. Prevention & Self-Care Tips
- Track cycles using apps (Clue, Flo, etc.).
- Maintain a balanced diet rich in iron and vitamin C.
- Stay hydrated and manage stress.
- Avoid abruptly stopping hormonal contraceptives.
- Get regular gynecological checkups.
12. Frequently Asked Questions (FAQ)
1. Is shedding the uterine lining painful?
Mild cramping is normal during menstruation. Severe pain could indicate hormonal imbalance, fibroids, or a decidual cast.
2. Can you see the uterus lining during your period?
Yes — small tissue fragments or mucus may be visible in menstrual blood. Large intact tissue, however, is not typical.
3. What does it mean if your period blood looks like skin or tissue?
It may be thicker endometrial tissue or clotted blood. If it’s large or shaped like an organ, see a doctor to rule out a decidual cast or miscarriage.
4. How long does it take for the uterus lining to rebuild?
Within a few days after menstruation ends, the lining starts regenerating and thickens through the proliferative phase.
5. Does hormonal birth control affect uterine lining shedding?
Yes. Hormonal contraceptives thin the endometrium and can reduce bleeding or stop periods altogether.
13. Summary
The uterine lining sheds naturally every month when pregnancy doesn’t occur. This shedding is part of a healthy menstrual cycle.
However, excessive bleeding, large tissue pieces, or severe pain may point to conditions like fibroids, adenomyosis, hormonal imbalance, or the rare decidual cast.
Monitoring your cycle and consulting a healthcare professional ensures early detection and proper treatment.
Healthy periods are a reflection of hormonal balance — listen to your body and seek help when something feels off.
References
- StatPearls: Physiology, Menstrual Cycle & Endometrial Function.
- FIGO Classification of Abnormal Uterine Bleeding (PALM-COEIN).
- Cleveland Clinic: Decidual Cast Causes and Treatment.
- Mayo Clinic: Abnormal Uterine Bleeding Overview.
- Merck Manual: Menstrual Disorders and Endometrial Physiology.