Decidual Cast vs Miscarriage: Key Differences, Symptoms, and When to Seek Help
Introduction
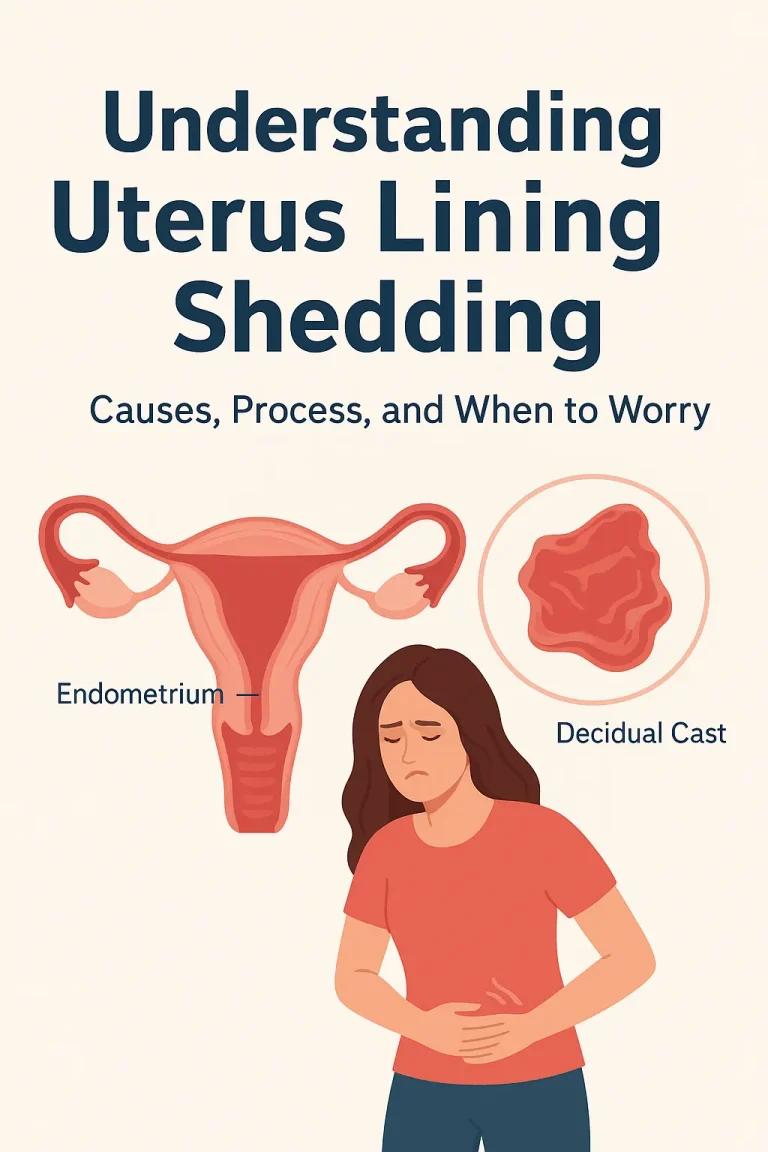
Passing tissue from the vagina can be an alarming experience, especially when it’s unclear whether it’s a decidual cast or a miscarriage. Both may involve pain, cramping, and visible tissue — but their causes, risks, and medical implications are very different.
Understanding how to distinguish the two can help you make informed decisions and seek appropriate care.
⚠️ Important: Only a healthcare professional can make a confirmed diagnosis through physical examination, ultrasound, and pregnancy testing.
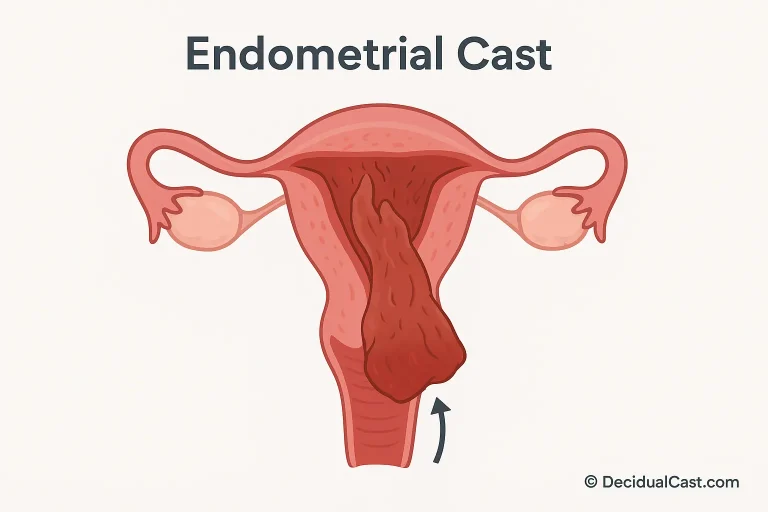
What Is a Decidual Cast?
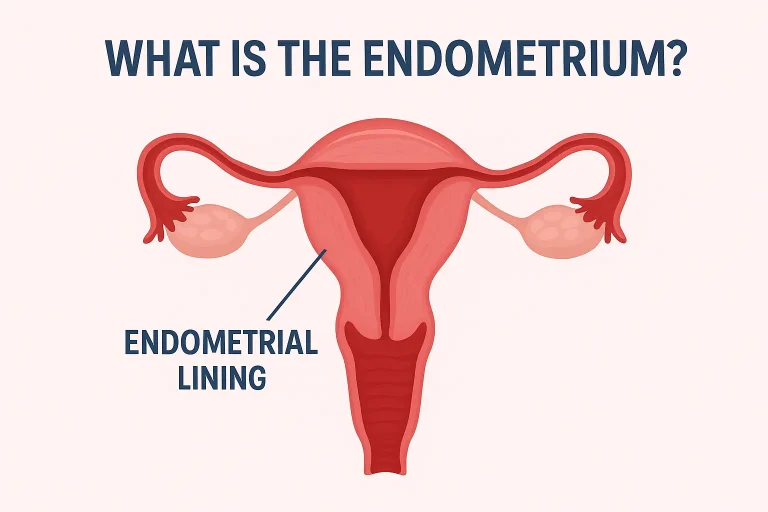
A decidual cast occurs when the entire uterine lining (decidua) is expelled in one piece, often maintaining the triangular shape of the uterus.
It typically happens due to hormonal imbalance, particularly when progesterone levels fluctuate suddenly — for instance, after using or stopping hormonal birth control.
Key Features of a Decidual Cast
- Tissue passes intact and may appear smooth, firm, or rubbery.
- Pain is sharp but short-lived; relief usually follows once tissue is expelled.
- Often linked to contraceptive hormones or non-pregnancy-related hormonal changes.
- Pregnancy tests are negative.
What Is a Miscarriage?
A miscarriage (spontaneous abortion) is the loss of a pregnancy before 20 weeks of gestation. It involves the expulsion of fetal or placental tissue along with the uterine lining.
Common causes include chromosomal abnormalities, hormonal insufficiency, or uterine structural issues.
Key Features of a Miscarriage
- Usually occurs after a positive pregnancy test.
- Tissue may include grayish, fleshy, or sac-like structures.
- Bleeding and pain may continue for several days.
- Emotional symptoms often accompany the event due to pregnancy loss.
Major Differences: Decidual Cast vs Miscarriage
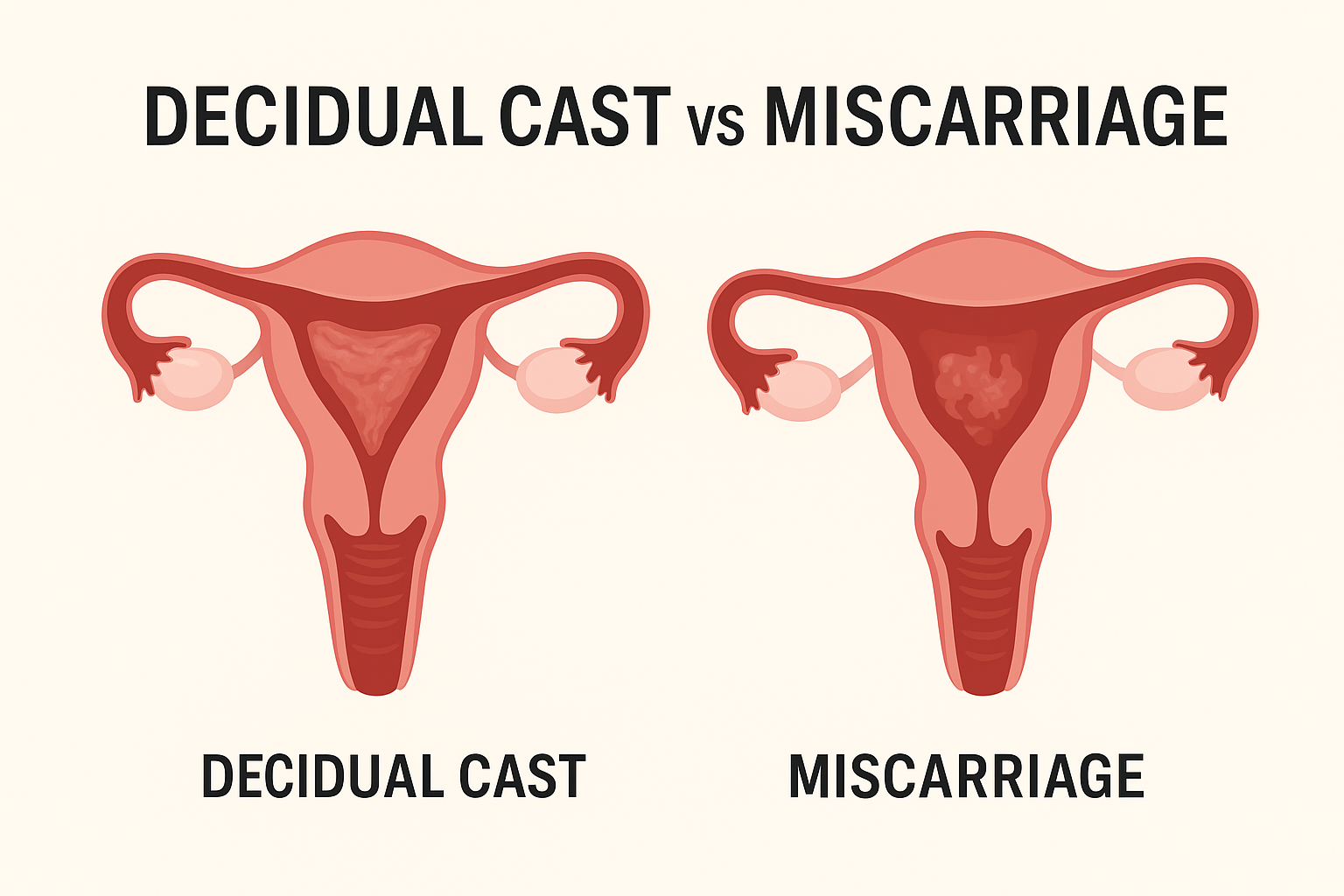
| Feature | Decidual Cast | Miscarriage |
|---|---|---|
| Cause | Hormonal imbalance, contraceptives | Loss of pregnancy (embryo or fetus) |
| Pregnancy Test | Negative | Positive |
| Tissue Type | Uterine lining (decidua) only | Pregnancy tissue (fetal + decidua) |
| Pain | Sharp, short-lived cramps | Prolonged cramping and back pain |
| Bleeding Duration | 1–3 days | Several days to weeks |
| Shape | Triangular, uterus-shaped | Irregular or sac-like |
| Emotional Impact | Shock, confusion | Grief due to pregnancy loss |
| Medical Urgency | Usually low | High – requires medical evaluation |
Diagnosis: How Doctors Tell the Difference
To confirm the cause, your healthcare provider may recommend:
- Pregnancy Test (hCG) – A positive result usually points toward a miscarriage.
- Ultrasound Scan – Identifies if pregnancy tissue remains or if uterine lining is normal.
- Pathology Analysis – Examining expelled tissue can confirm whether embryonic cells are present.
- Hormonal History Review – Recent birth control or hormonal therapy may explain decidual shedding.
🩺 Note: Bring the expelled tissue (if possible) in a sterile container for analysis. It can help doctors make a precise diagnosis.
When to Seek Medical Help
You should always seek urgent medical attention if you experience:
- Heavy bleeding (soaking more than one pad per hour)
- Severe or persistent pain
- Dizziness or fainting
- Positive pregnancy test before the event
- Foul-smelling vaginal discharge or fever
Even if it turns out to be a decidual cast, ruling out ectopic pregnancy or incomplete miscarriage is essential.
Emotional and Physical Recovery
Both experiences can be distressing — physically and emotionally.
- Rest and hydrate well after the event.
- Avoid inserting anything into the vagina (like tampons) until cleared by a doctor.
- Seek emotional support or counseling if you experience anxiety or grief.
If it was a miscarriage, discuss with your healthcare provider about future pregnancy planning and prenatal care.
If it was a decidual cast, a hormonal review may help prevent recurrence.
FAQs
Q1: Can a decidual cast happen during pregnancy?
Rarely, yes — sometimes during an ectopic pregnancy. Always get checked immediately if pregnancy is suspected.
Q2: What does a decidual cast look like compared to miscarriage tissue?
A decidual cast often looks like a hollow, uterine-shaped mold. Miscarriage tissue may contain irregular parts, sacs, or grayish material.
Q3: Can I have both — a miscarriage and a decidual cast?
It’s uncommon but possible in certain cases of ectopic or abnormal pregnancy. Medical evaluation is crucial.
Conclusion
Although both a decidual cast and a miscarriage involve the passage of tissue, their causes, implications, and emotional impacts are distinct.
A negative pregnancy test often indicates a decidual cast, while a positive test with persistent bleeding points to a miscarriage.
When in doubt, always consult your gynecologist for a full evaluation — early medical guidance can prevent complications and offer peace of mind.