Decidual Cast vs Blood Clot: Clinical Differences, Diagnosis & Management
Overview
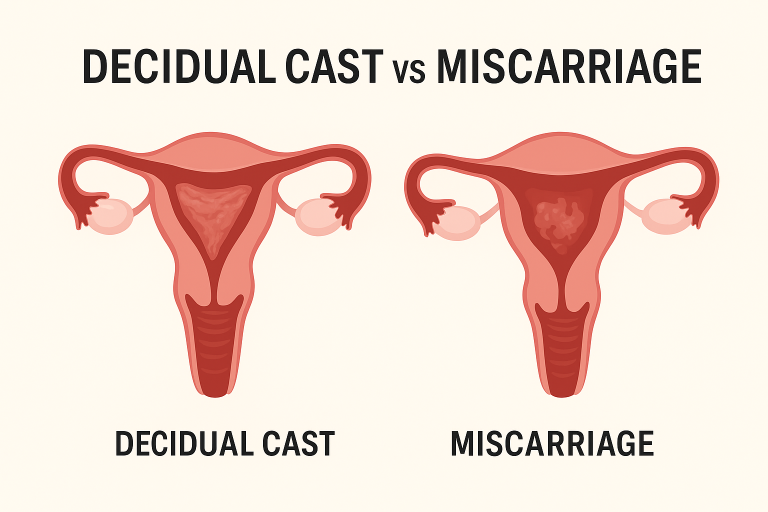
Passing tissue or clots per vagina may be alarming. Two commonly conflated entities are the decidual cast (also described as an endometrial cast or membranous dysmenorrhea) and routine menstrual blood clots. Clinically, the distinction is based on structure, composition, etiology, and the associated diagnostic findings. This article summarizes the evidence-based approach to differentiate decidual cast vs clot, appropriate evaluation (hCG, ultrasound, histology), and recommended management steps.
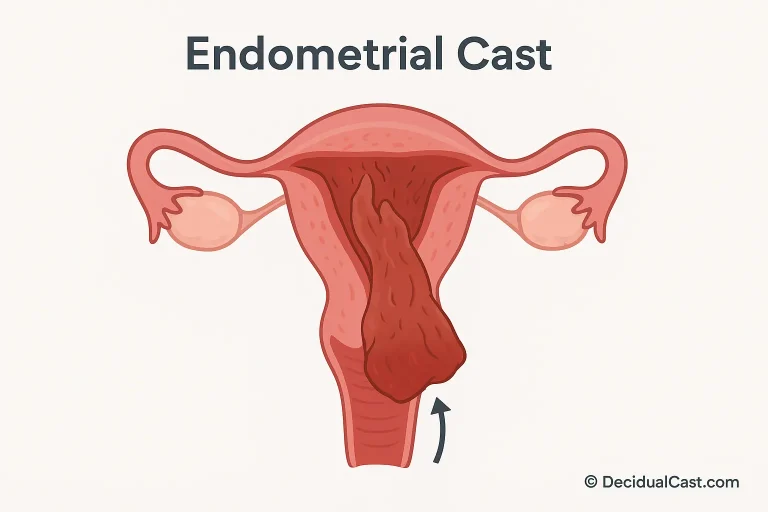
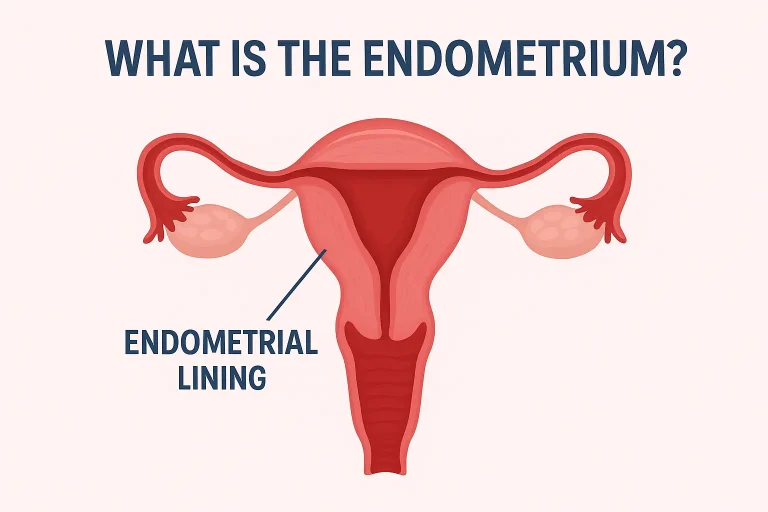
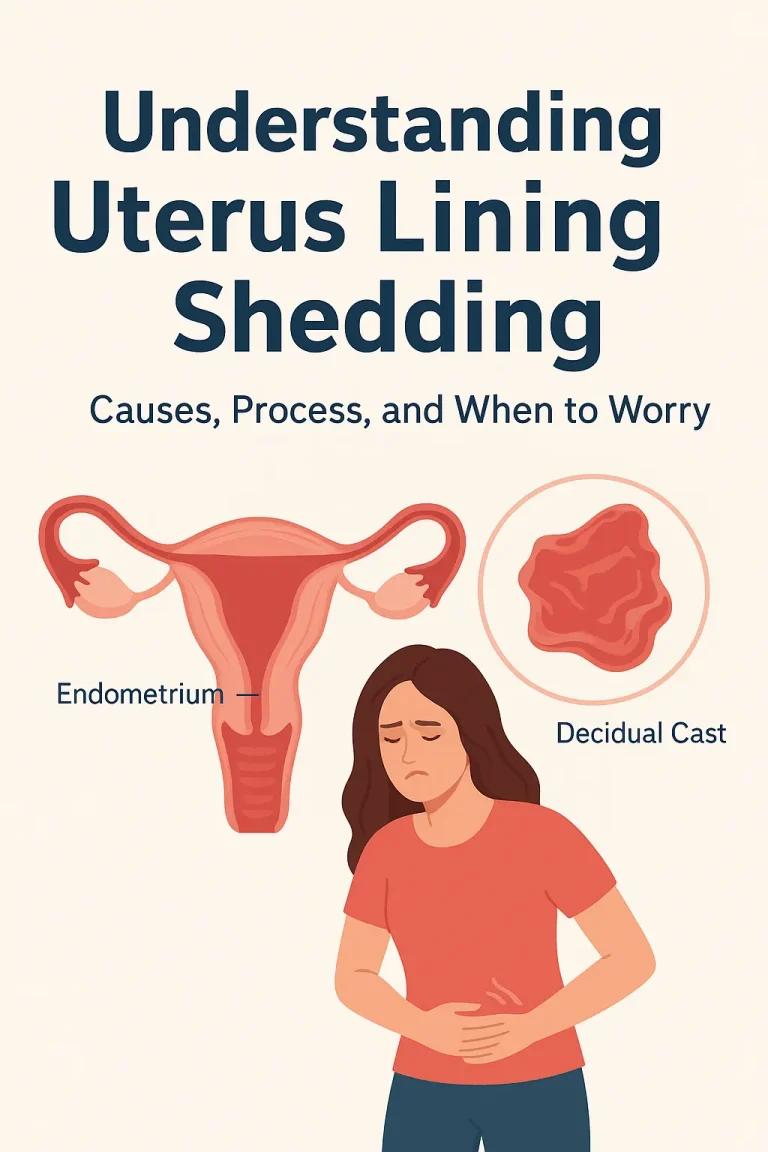
What Is a Decidual Cast?
A decidual cast is the en bloc expulsion of the uterine lining (decidua/endometrium) as an intact piece that often retains the internal morphology of the uterine cavity. It is a distinct clinical entity from fragmented menstrual debris and is most often associated with abrupt hormonal changes or, rarely, pregnancy-related processes.).
What Is a Menstrual Blood Clot?
A menstrual blood clot results from blood pooling and coagulation within the uterine cavity before expulsion. Clots are typically amorphous, gelatinous and lack organized uterine structure. Large clots are common with heavy menstrual bleeding and are thoroughly reviewed by sources such as Healthline and the Mayo Clinic.
Clinical Comparison: Decidual Cast vs Clot
Below is a concise clinical comparison that highlights key differentiators relevant to diagnostic reasoning.
| Feature | Decidual Cast | Menstrual Clot |
|---|---|---|
| Composition | Organized endometrial tissue (decidua) | Coagulated blood +/- fragmented tissue |
| Appearance | Triangular / uterus-shaped, fleshy, rubbery | Amorphous, jelly-like, fragmentary |
| Typical cause | Hormonal withdrawal, progestin effects, rare pregnancy association | Normal menstrual shedding, heavy flow etiologies |
| Associated tests | hCG to exclude pregnancy; ultrasound; histopathology | No pregnancy implication; ultrasound if abnormal bleeding |
| Urgency | Low once pregnancy/ectopic excluded; evaluate for retained tissue | Usually benign; evaluate if menorrhagia or anemia |
Etiology & Risk Factors
Documented triggers include abrupt progesterone withdrawal, initiation or cessation of progestin-based contraception (eg, injectable progestins, implants, IUDs), and exogenous hormone regimens used in fertility treatment. Rarely, decidual casts have been reported in association with early pregnancy loss or ectopic gestation. A clinical review of case reports and series is available via Medical News Today.
Presentation & Symptoms
Typical clinical features include an episode of severe cramping immediately preceding passage, followed by expulsion of a single intact tissue mass and rapid symptomatic relief. Associated findings can include transient lightheadedness or heavier bleeding during the event. Persistent fever, prolonged bleeding, or hemodynamic instability necessitate urgent assessment.
Diagnostic Approach (Evidence-Based)
The diagnostic workflow should be methodical:
- Pregnancy test (urine or serum β-hCG) — immediately rule out intrauterine or ectopic pregnancy.
- Transvaginal ultrasound — evaluate for retained products, uterine anomalies, or adnexal pathology.
- Histopathologic analysis of expelled tissue when available — confirms decidualized endometrium versus embryonic tissue. Case literature with histology is available in PMC reports. (PMC case report).
- Laboratory tests — CBC for anemia, inflammatory markers if infection suspected.
Management & Follow-up
Management is typically conservative unless complications are present. Recommended actions:
- Supportive care: analgesia (NSAIDs), hydration and rest.
- Follow-up ultrasound if bleeding persists or if physical exam suggests retained tissue.
- Antibiotic therapy if clinical or laboratory evidence of infection.
- Surgical uterine evacuation only if imaging confirms retained products or ongoing significant hemorrhage.
If the event is temporally associated with changes in hormonal contraception, refer to the prescribing clinician for regimen reassessment to mitigate recurrence risk.
When to Seek Urgent Care
Immediate evaluation is indicated for: hemodynamic instability (syncope, hypotension), ongoing heavy bleeding (soaking ≥1 pad/hour), positive pregnancy test with tissue passage, fever >38°C or purulent discharge, or severe unrelieved abdominal pain. These signs warrant emergency assessment to exclude ectopic pregnancy, retained products, or sepsis.
Patient Counseling Points
Counsel patients that a single decidual cast is usually self-limited and does not typically affect long-term fertility. Encourage cycle tracking, documentation of events (photograph or retain tissue in a clean container if safe), and early contact with a clinician for any concerning symptoms. Provide reassurance while emphasising the importance of appropriate diagnostic testing.
Frequently Asked Questions
How do clinicians differentiate a decidual cast from a clot?
Differentiation relies on clinical history, physical inspection of expelled tissue (if available), pregnancy testing, ultrasound imaging, and histopathology. The intact uterus-shaped morphology and histologic confirmation of decidualized endometrium indicate a decidual cast.
Does passing a decidual cast mean I was pregnant?
Not necessarily. Decidual casts can occur in non-pregnant individuals, often after hormonal changes. However, any passage of tissue should prompt pregnancy testing to exclude miscarriage or ectopic pregnancy.
Will a decidual cast affect my fertility?
Most individuals resume normal menstrual function and fertility; persistent menstrual irregularities should prompt endocrinologic and gynecologic assessment.