Decidual Cast IUD (Intrauterine Devices)
Introduction
If you use an intrauterine device (IUD), you may have read about or heard of a decidual cast — a rare occurrence in which the lining of the uterus is expelled in a single piece. While extremely uncommon, understanding how an IUD may influence this process can give you clarity, reduce anxiety, and help you make informed choices about your contraceptive method and menstrual health.
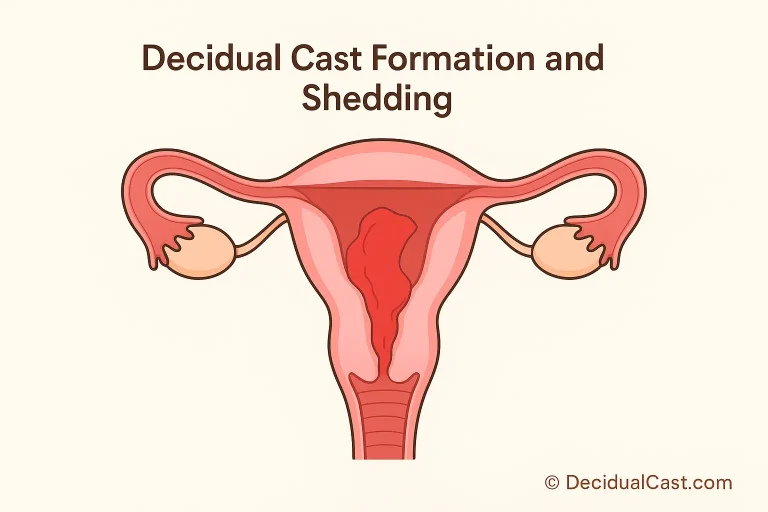
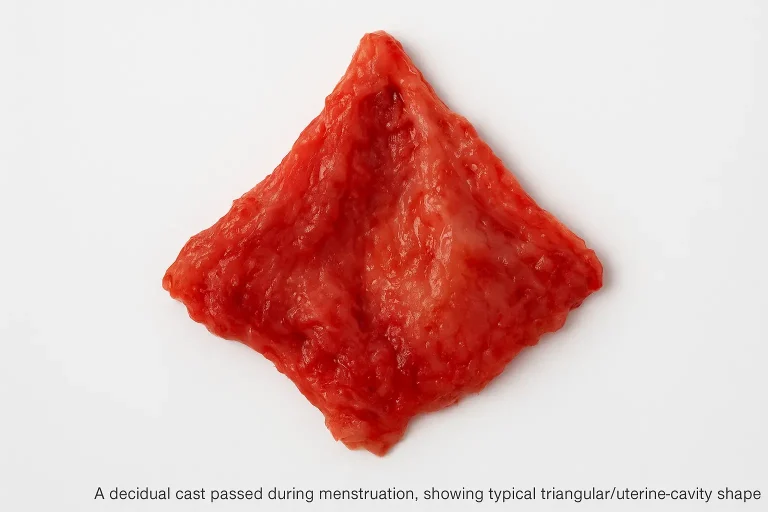
A decidual cast (also called membranous dysmenorrhea) occurs when the uterine lining (endometrium) becomes decidualized — thickened under the influence of progesterone — and then is shed in one solid piece, rather than the normal gradual breakdown and discharge during menstruation.
The expelled tissue often retains the shape of the uterine cavity, forming a triangular or light-bulb-shaped “cast.”
How IUDs May Be Linked to a Decidual Cast
Hormonal IUDs
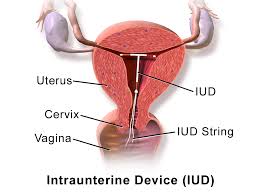
Hormonal IUDs (e.g., levonorgestrel-releasing) deliver progestin locally, which thins the endometrium and often suppresses bleeding. In some cases, this altered endometrial environment may predispose to a decidual cast — particularly if there are abrupt hormonal changes or the lining responds in an unusual way.
Copper (Non-Hormonal) IUDs
Copper IUDs provoke an inflammatory response in the endometrium (foreign body reaction) and may alter how the lining sheds. While a rarer association, this inflammatory milieu could theoretically influence abrupt shedding of the uterine lining.
What the Research Shows
- A case report described a 13-year-old adolescent who developed a decidual cast shortly after stopping an oral contraceptive; hormone withdrawal played a role rather than IUD per se.
- There are individual reports from IUD users who passed a piece of tissue resembling a decidual cast shortly after IUD insertion (for example in Reddit discussions) but large-scale data are lacking.
What this means in practice
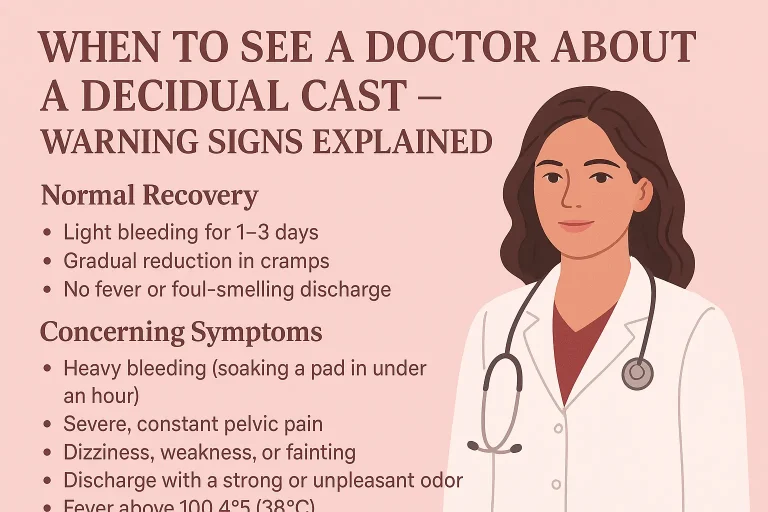
Using an IUD does not guarantee a decidual cast will occur, nor is a cast a definitive side effect of all IUD use. But if you’re a user and experience unusual tissue passing, heavy bleeding, or severe cramping, you should discuss it with your provider.
Symptoms & Warning Signs in IUD Users
If you have an IUD and pass tissue that might be a decidual cast, symptoms may include:
- Sudden severe cramping, more intense than your usual period
- Passage of a fleshy tissue mass, often triangular/uterus-shaped
- Heavy bleeding or abrupt onset of flow
- Nausea, dizziness, or feeling faint
- In the context of IUD use: these events may occur shortly after insertion, after changing method, or after a hormonal shift
It’s especially important to evaluate if you are pregnant or could be pregnant, since some symptoms overlap with miscarriage or ectopic pregnancy.
Diagnosis & What Your Clinician Will Check
With an IUD present, the diagnostic work-up usually includes:
- Pregnancy test (β-hCG): Must rule out intrauterine or ectopic pregnancy.
- Pelvic / transvaginal ultrasound: Check IUD position, retained tissue, uterine abnormalities.
- History of contraceptive method: Type of IUD (hormonal/copper), length of use, any recent changes.
- Tissue analysis (if available): If you saved or photographed the tissue passed, histopathology may confirm decidualized endometrium.
- Hormonal and bleeding profile: Particularly if recurrences occur, check for underlying menstrual/ovarian pathology.
Management & Guidance for IUD Users
- Immediate care: For pain and bleeding, use NSAIDs, apply heat, rest, and keep hydrated.
- IUD evaluation: Ensure that the IUD is properly placed and has not caused mechanical irritation or uterine change (which may contribute).
- Alternative methods: If the decidual cast is strongly linked with hormonal IUD use (especially in your history of heavy cramping/bleeding), you may discuss switching to non-hormonal method or lower dose hormonal option.
- Monitor future cycles: Keep a menstrual/bleeding diary post‐event. If recurrence occurs, a specialist referral may be needed.
- Reassurance: Most cases do not lead to serious complications or compromise fertility.
FAQs: Decidual Cast & IUDs
Q1. Can an IUD cause a decidual cast?
A1. An IUD, especially hormonal progestin-releasing ones, may alter the endometrial lining and in rare instances contribute to a decidual cast. However, a causative link in all users has not been proven; many other factors (hormonal shifts, contraceptive changes, pregnancy status) are involved.
Q2. If I pass tissue with my IUD in place, is it a miscarriage?
A2. Not necessarily. A decidual cast is uterine lining tissue, not pregnancy tissue. But because symptoms overlap with miscarriage or ectopic pregnancy, you should do a pregnancy test and contact your clinician.
Q3. Should I remove my IUD after passing a decidual cast?
A3. Not automatically. You should have the IUD evaluated for correct placement and the cause of bleeding/cramping discussed with your provider. Removal or method change may be considered if recurrence or heavy symptoms persist.
Q4. Does a decidual cast affect future fertility in an IUD user?
A4. There is currently no evidence that a single decidual cast event impairs fertility. If you are concerned, discuss further evaluation with a fertility specialist.
Q5. How can I reduce the risk of a decidual cast while using an IUD?
A5. While you cannot completely prevent it (because the exact cause is unclear), strategies include: tracking your cycle, promptly evaluating any unusual bleeding/cramping, selecting the most appropriate IUD type for your body and hormonal profile, and discussing changes in contraceptive method with your clinician.
Conclusion
For individuals using an IUD, experiencing a decidual cast can be surprising and frightening — especially when large tissue passes, or the event mimics other conditions. The key steps are: stay calm, do a pregnancy test, keep the tissue/photo if possible, and consult your clinician. Most IUD users who experience this do not have serious complications, and the event alone does not necessarily warrant abandoning the IUD. Awareness, monitoring, and clinical follow-up are your best tools in managing this rare phenomenon.