Endometrial Cast vs Decidual Cast: What’s the Difference?
When patients present with unusual bleeding and the passage of tissue, two very rare but distinct phenomena may be considered: an endometrial cast and a decidual cast. While both involve the shedding of uterine-lining tissue, their causes, appearance, clinical implications and management differ significantly. As a women’s health specialist, I’ll guide you through the subtleties between these two events — what they are, how to differentiate them, how they are diagnosed, and how we approach treatment and care.
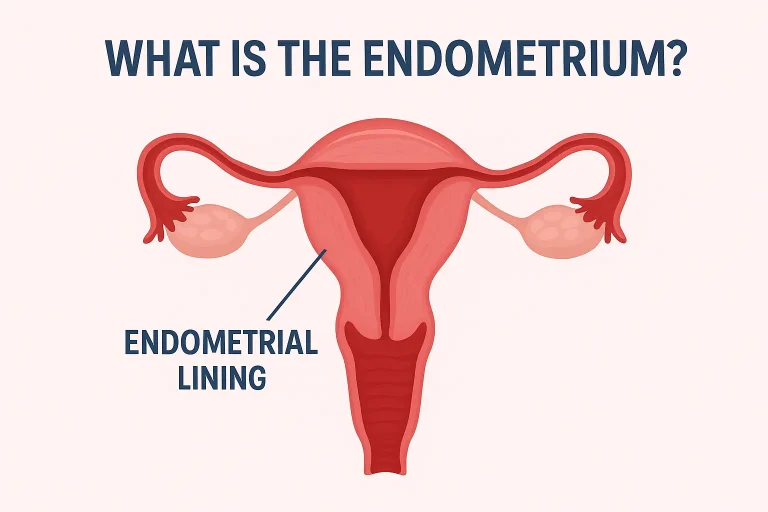
What Is an Endometrial Cast?
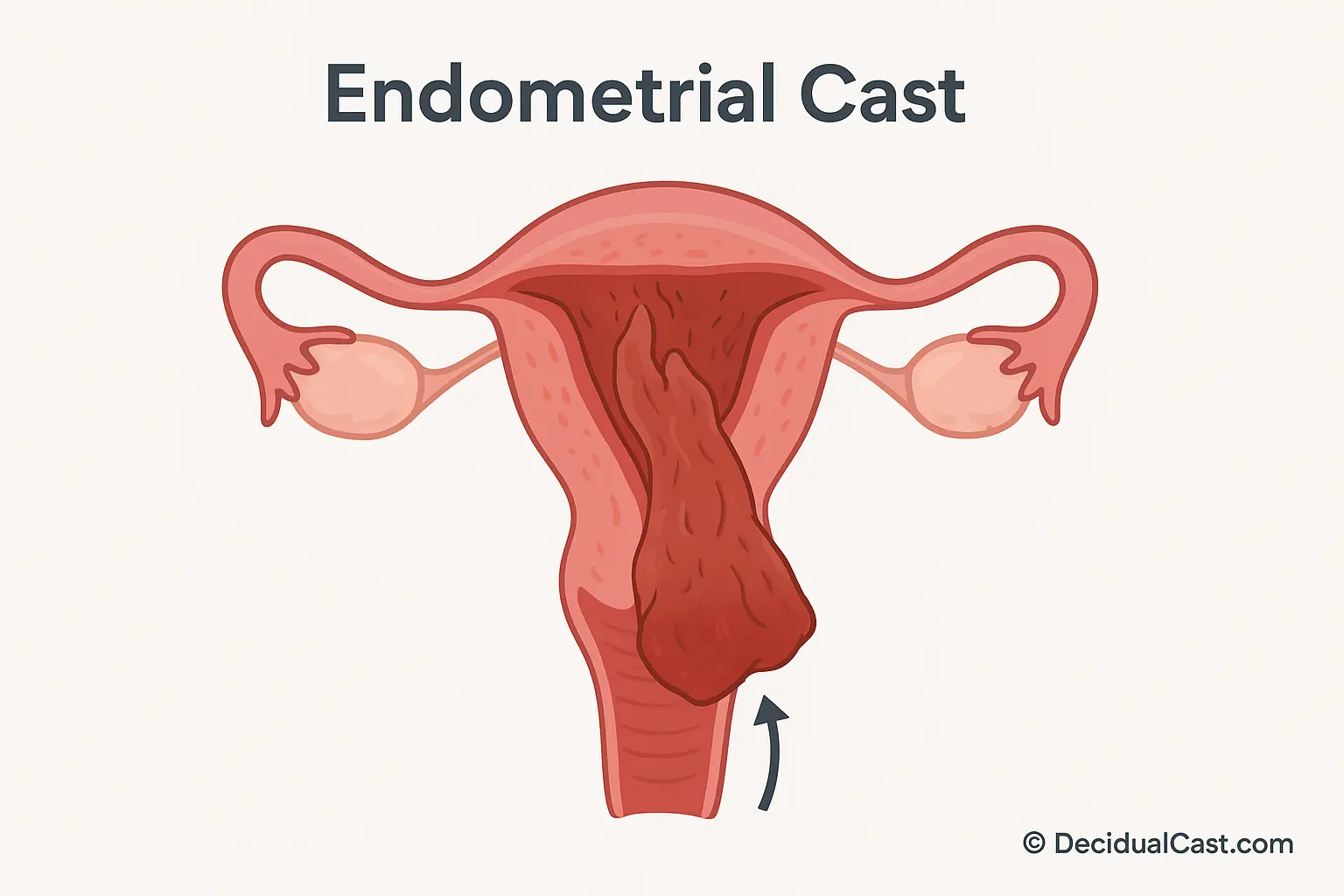
An endometrial cast refers to the shedding of nearly the entire functional lining of the uterus (endometrium) in one piece, rather than the usual gradual shedding seen in a standard menstrual period. In this scenario, the expelled tissue may approximate the shape of the uterine cavity, though often less perfectly so than in a decidual cast. According to case reports, this phenomenon is sometimes labelled “membranous dysmenorrhea” when it occurs with pain and distinctive tissue passage.
Clinically, a woman may notice passing a larger-than-expected tissue fragment or mass during menstruation or abnormal bleeding — something that looks more like a sac of lining than typical clots. That tissue often consists of endometrial glands, stroma, and blood vessels, and may retain the morphology of the uterine cavity to some degree.
Because endometrial casts are extremely rare, many women and even clinicians may not immediately recognize the event. It is distinguished from more common processes such as large blood clots or retained products of conception. One documented case described a teenager who passed a tissue that maintained the shape of the uterus after being on hormonal therapy. For the clinician, suspicion arises when the tissue appears unusually intact and the level of pain and passage is more dramatic than typical menstruation.
In short: an endometrial cast is the large-volume, intact shedding of the uterine lining in a single piece, outside of the usual menstrual fragmentation.
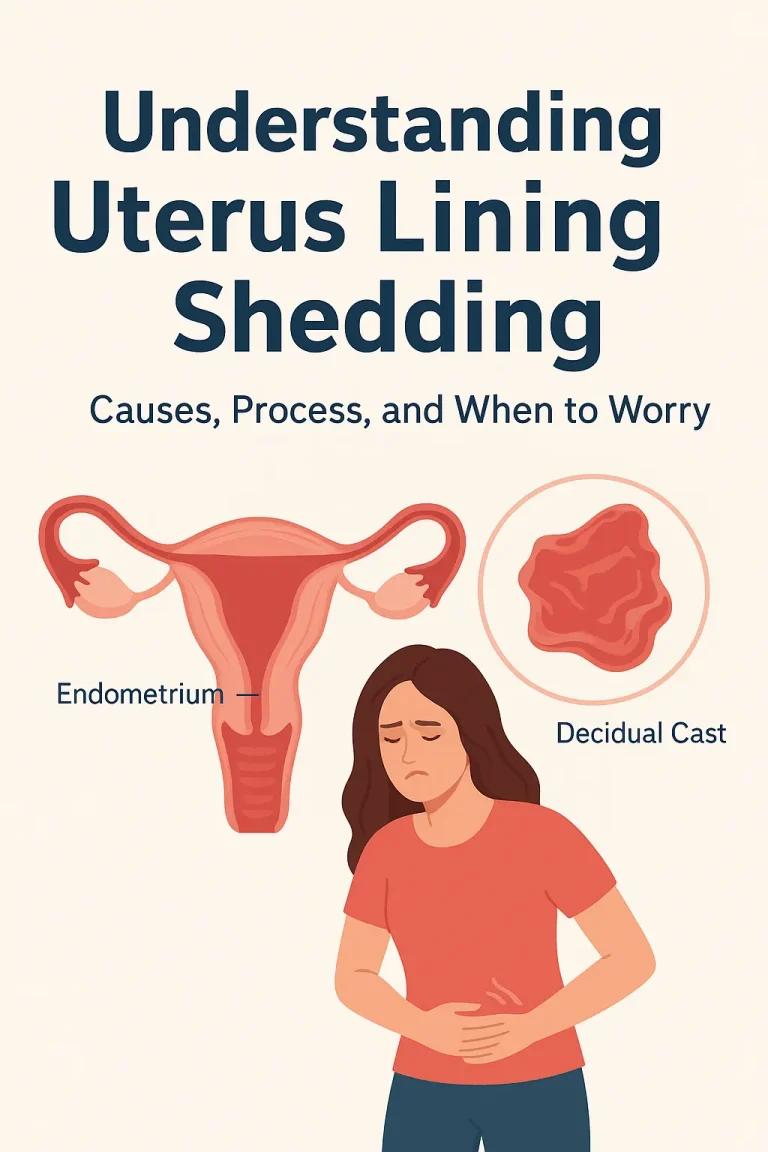
What Is a Decidual Cast?
While we just described an endometrial cast, a decidual cast is a closely related but distinct entity. In a decidual cast, the lining that has undergone decidualization (that is, the uterine lining modified in response to progesterone and prepared for possible pregnancy) is expelled in one piece.
In practical terms: the functional endometrium becomes decidualized (for instance under hormonal influence or early pregnancy), and then, instead of gradual shedding, the entire layer is shed as a triangular or inverted-triangle piece shaped like the uterine cavity. Symptoms often include acute, intense cramping and the passage of a fleshy mass. While not inherently dangerous, a decidual cast may signal more serious underlying issues like ectopic pregnancy or hormone-driven changes.
→ See full article: “What Is a Decidual Cast?”
So: whereas both involve intact tissue expulsion, the key distinction is that a decidual cast involves decidualized endometrium (prepared for pregnancy) whereas an endometrial cast may not.
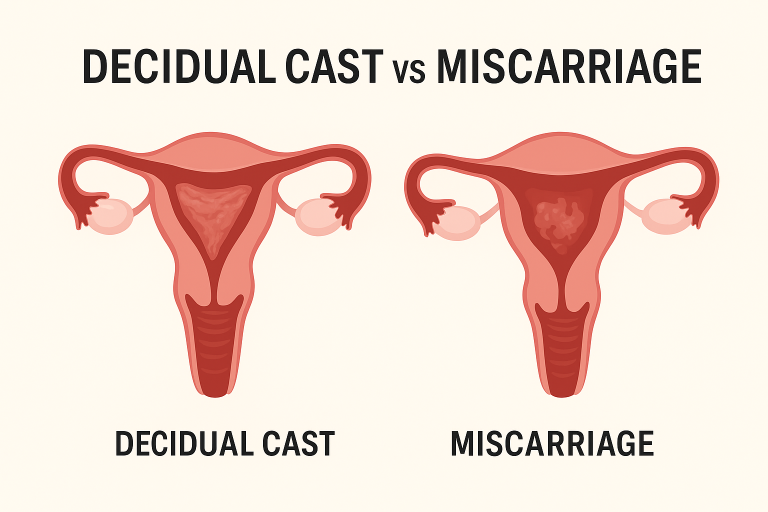
Visual and Structural Differences
From a clinical perspective, recognising the differences between an endometrial cast and a decidual cast is important. Here are how they compare in appearance and structure:
| Feature | Endometrial Cast | Decidual Cast |
|---|---|---|
| Tissue origin | Endometrial lining (functional layer) | Decidualized lining (modified by progesterone/pregnancy) |
| Shape and size | Often large, may resemble cavity but less perfectly cast | Typically retains uterine-cavity shape (triangle/inverted V) |
| Colour and texture | May look tan-pink, mixed with blood and clots | Often fleshy, red/pink, thick, sometimes shiny appearance |
| Associated pain | May be painful, depending on volume and passage | Frequently very painful due to the size and intact pass |
| Typical context | Heavy menstrual bleeding, hormonal changes | Pregnancy-related changes, hormonal preparation, ectopic risk |
| Clinical implication | Rare, but often benign unless associated with other pathology | Rare; may signal ectopic pregnancy or hormonal shifts |
For example, a woman who passes a large triangular piece of tissue after intense cramping may well have experienced a decidual cast. In contrast, someone on hormonal therapy who passes a bulky piece of lining during what seemed like an exaggerated period may have an endometrial cast.
Visual clues such as the intact shape of the uterine cavity, and the texture (fleshy vs granular/clot-like) help differentiate. The medical term often applied is membranous dysmenorrhea for both phenomena when accompanied by severe pain.
Common Causes of Each
Endometrial Cast – Causes
The roots of an endometrial cast are not fully understood, but several contributing factors include:
- Rapid hormonal shifts: Sudden withdrawal of progesterone or estrogen may destabilize the lining and trigger one-piece shedding.
- Progestin-only contraceptives: Some case reports link hormonal contraceptives to cast formation, possibly through altering the endometrial maturation.
- Structural variance: A thicker than normal lining, due to adenomyosis or hyperplasia, may predispose to sloughing en-bloc.
- Uterine contractility: Intense contractions may help expel the tissue intact rather than in pieces.
Decidual Cast – Causes
Decidual casts are more widely documented and the known associations are:
- Decidualized lining: Occurs when progesterone has transformed the endometrium (as in early pregnancy or with progestin therapy).
- Ectopic pregnancy: A crucial cause to rule out — the lining may shed even though the pregnancy is outside the uterus.
- Hormonal contraceptives: Particularly progestin-based implants, injections or pills have been associated.
- Pregnancy loss: In some cases the cast may follow very early pregnancy failure, though the cast is not itself a miscarriage.
- Membranous dysmenorrhea mechanism: The intact mass passing through an undilated cervix causes significant pain.
Because the decidual cast involves a lining prepared for pregnancy, when it occurs in a non-pregnant state, it signals a rapid change in hormonal environment or other disruption of normal endometrial physiology.
Related Post: causes of decidual cast
How Doctors Diagnose Casts
When a woman reports passing tissue and intense cramping or unusual bleeding, the clinician’s approach is systematic:
- History & Symptoms: When did bleeding occur, what was the tissue like, were there signs of pregnancy?
- Pregnancy test: Very important, because an ectopic pregnancy can mimic or accompany a cast.
- Pelvic examination & ultrasound: To assess retained tissue, uterine shape, and rule out masses or pregnancy.
- Examine the tissue (if available): The patient may bring the expelled tissue in a container for gross evaluation.
- Lab tests: Blood counts for anemia, infection markers, coagulation if heavy bleeding.
- Differential diagnosis: Consider miscarriage, retained products, fibroids, polyps, or sarcoma.
- Follow-up imaging: If ultrasound is inconclusive, further imaging or hysteroscopy may be considered.
For example, in a confirmed decidual cast case, the ultrasound may show no remaining intrauterine tissue and the pregnancy test negative. In both endometrial and decidual cast work-ups, once dangerous causes are ruled out, the management becomes supportive.
Treatment and Care Options
Immediate Care
- Pain management: Strong cramps often accompany the passage of a cast. Use NSAIDs (ibuprofen) and apply heat to the lower abdomen.
- Monitor bleeding: If bleeding is very heavy (soaking a pad/hour), seek urgent care.
- Observation: If the cast has passed entirely and no retained tissue is seen on ultrasound, often no further intervention is required.
Specific Considerations
- For endometrial cast: If associated with hormonal contraceptive initiation or withdrawal, review the contraceptive regimen with your clinician. If abnormal uterine bleeding was present, evaluate for underlying uterine pathology (hyperplasia, fibroids).
- For decidual cast: Given the association with ectopic pregnancy or early loss, careful follow-up is required. The clinician might perform serial hCG levels if pregnancy was possible. Also, review any hormonal therapy or contraceptive usage.
Long-Term Follow-up
- Evaluate for underlying causes: Hormone levels, uterine imaging, coagulopathy if bleeding was extreme.
- Lifestyle support: Healthy weight, balanced hormones, regular menstrual patterns help prevent irregular shedding.
- Counselling: Because the event can be alarming, reassure patients — both endometrial and decidual casts rarely lead to long-term problems, although recurrence may occur in some cases.
Related: When to See Your OBGYN About a Decidual Cast
FAQs
Are endometrial and decidual casts the same?
No — while both involve the passage of large pieces of uterine lining, an endometrial cast is the shedding of the uterine lining in a mostly unmodified state, whereas a decidual cast involves a decidualized lining (modified for pregnancy) and typically occurs in different clinical contexts.
Which one is more painful?
Pain intensity often correlates with the volume and the intactness of the tissue being expelled plus uterine contractility. Decidual casts tend to be more acutely painful due to their larger size and the fact that the cervix may not be dilated. Endometrial casts can also be very painful depending on individual circumstances, but the literature suggests decidual casts more consistently present with intense cramps.
Conclusion
In women’s reproductive health, the sight of a large tissue mass or “cast” emerging from the uterus is understandably disruptive and frightening. Differentiating between an endometrial cast and a decidual cast matters, because their underlying causes, implications and follow-up differ. With careful history, pregnancy testing, imaging, and patient-centred care, most cases can be managed with reassurance, pain relief and monitoring. As with all unusual bleeding or tissue passage, prompt medical evaluation ensures safety, peace of mind, and optimal reproductive health.