When to See a Doctor About a Decidual Cast?
Key Takeaways
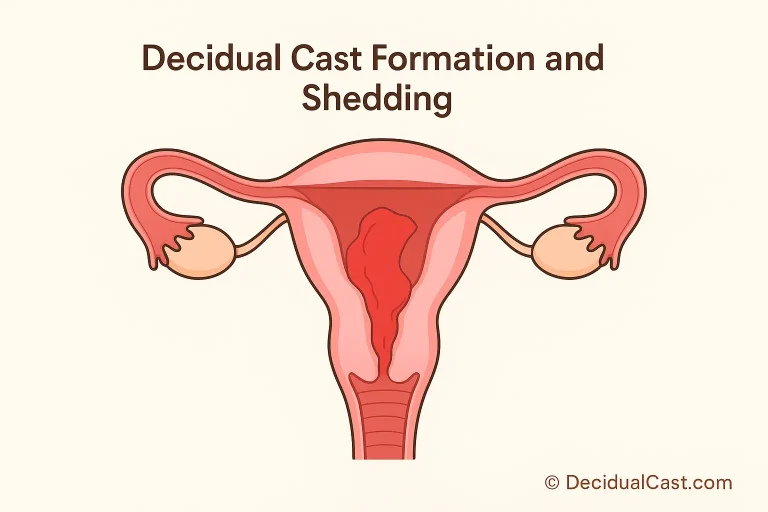
- A decidual cast forms when the entire uterine lining sheds at once — often due to sudden hormonal shifts.
- See your doctor immediately if you notice severe pain, heavy bleeding, fever, or foul-smelling discharge.
- Mild symptoms that resolve within a few days may not require emergency care, but a check-up is still recommended.
- Gynecologists diagnose possible causes using ultrasound, pelvic exams, or hormone testing.
- Follow-up care may include adjusting birth control, treating infection, or monitoring hormone balance.
- When in doubt, seek professional advice — especially if you’re unsure whether what you passed was a decidual cast or another type of tissue.
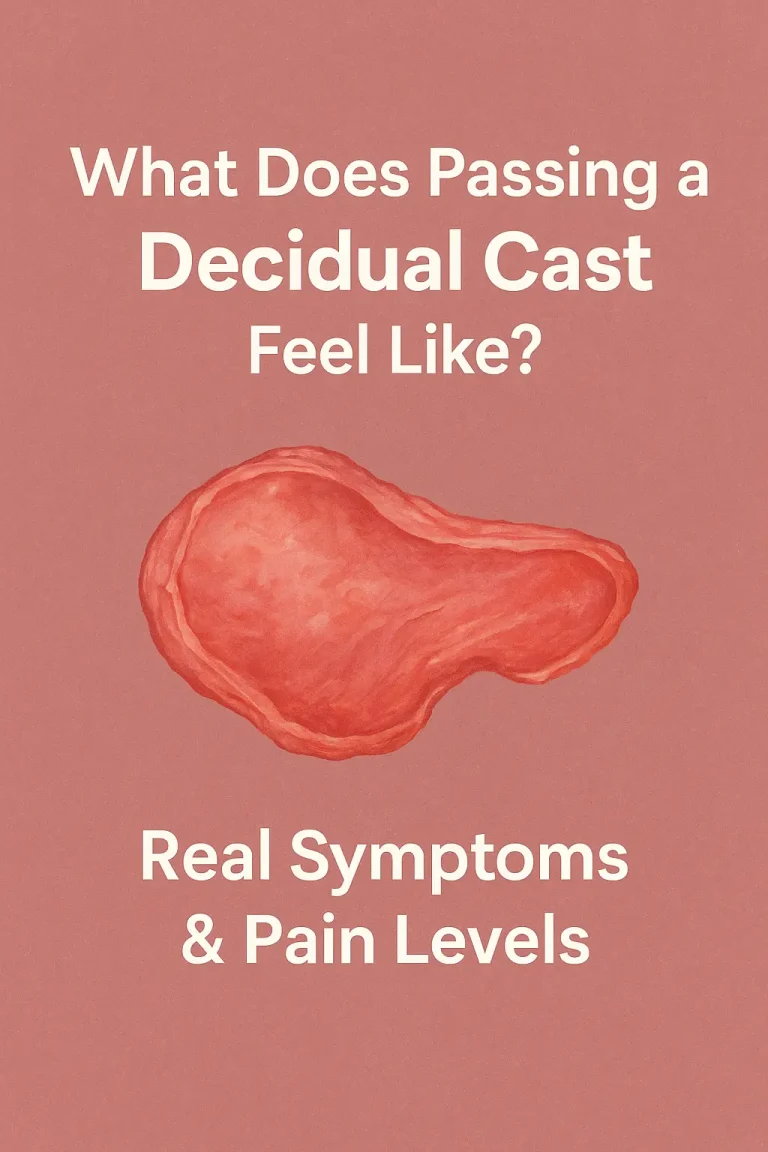
Passing a decidual cast can be a shocking experience — the sudden discharge of a large, tissue-like mass from the uterus often causes confusion and concern. While this phenomenon is rare and sometimes harmless, it can also indicate an underlying issue such as hormonal imbalance, birth control side effects, or uterine inflammation.
Knowing when to see a doctor after passing a decidual cast is crucial for your reproductive health. In many cases, mild cramping and brief bleeding resolve on their own. However, if you experience severe pain, heavy bleeding, fever, or unusual discharge, it’s time to contact your OBGYN for evaluation.
This article explains how to recognize warning signs that need medical attention, what to expect during your doctor’s appointment, and how proper follow-up care helps prevent recurrence.
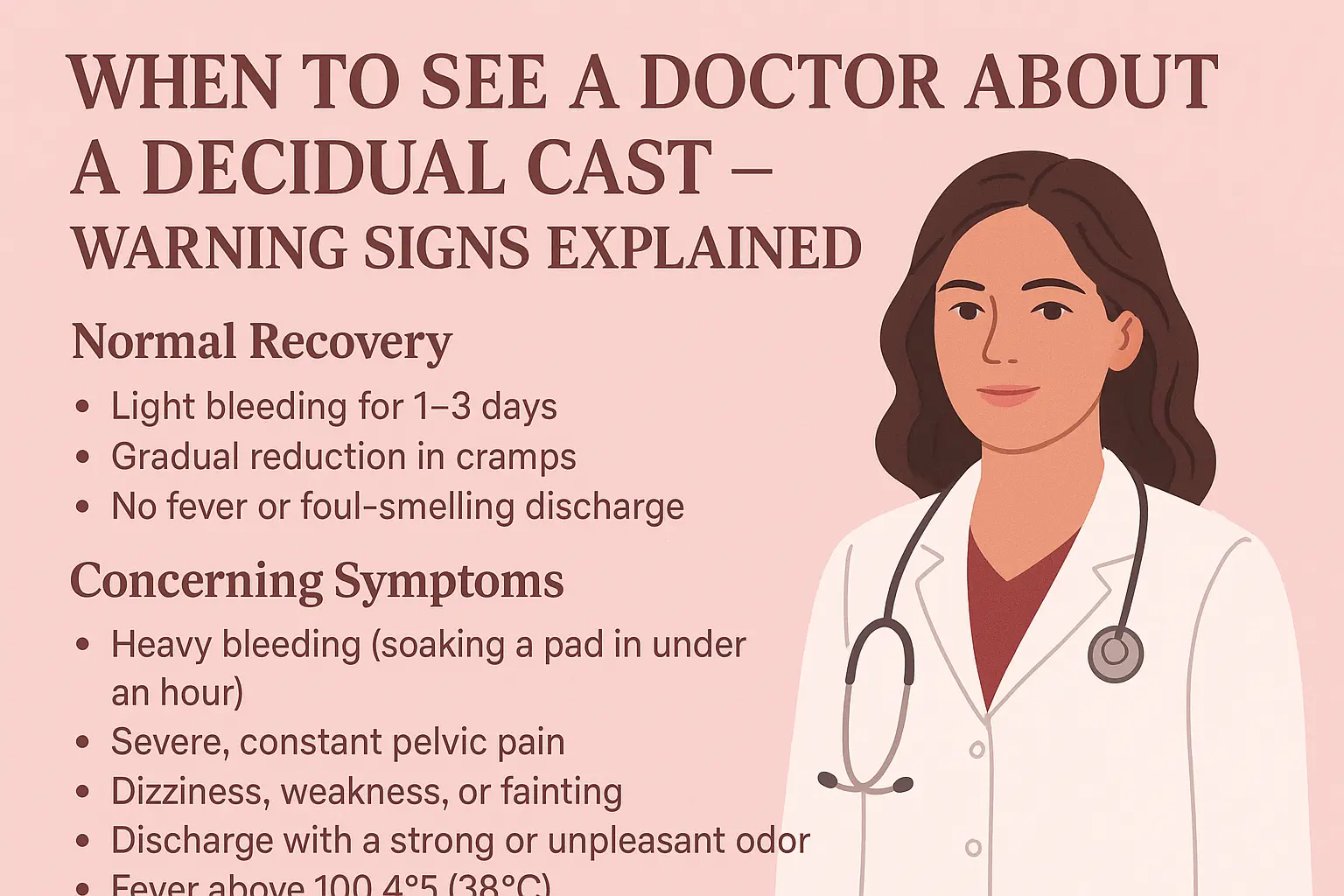
Normal recovery signs:
- Light bleeding for 1–3 days
- Gradual reduction in cramps
- No fever or foul-smelling discharge
Warning signs:
- Heavy bleeding (soaking a pad in under an hour)
- Severe, constant pelvic pain
- Dizziness, weakness, or fainting
- Discharge with a strong or unpleasant odor
- Fever above 100.4°F (38°C)
If you notice any of these, medical evaluation is essential to rule out infection or incomplete tissue passage.
When Medical Help Is Necessary
You should see your OBGYN or gynecologist immediately if:
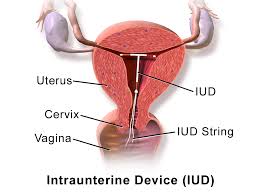
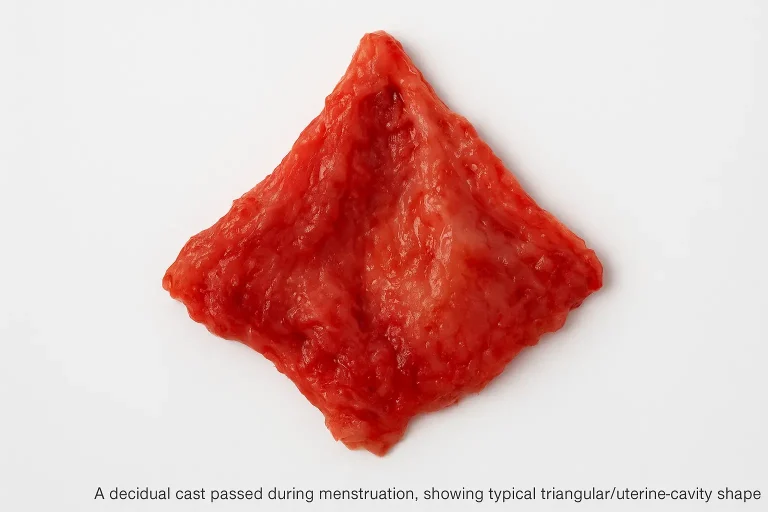
- You pass tissue larger than a golf ball or shaped like the inside of your uterus
- The pain is sharper or stronger than typical menstrual cramps
- You’ve recently changed or stopped birth control or hormonal medication
- You experience irregular cycles or missed periods afterward
Even if the symptoms subside, a follow-up visit ensures your uterus has healed properly and no complications remain.
How Doctors Diagnose Uterine Conditions
During your visit, the doctor may perform:
- Pelvic exam – to check for tenderness or infection
- Ultrasound – to confirm if all tissue has been expelled
- Blood tests – to check hormone levels or possible pregnancy-related issues
- Medical history review – including medications and recent cycle changes
These steps help your doctor confirm whether it was a decidual cast or a different uterine condition, such as a miscarriage or fibroid shedding.
What to Expect During the Appointment
Your doctor may ask about:
- When your symptoms started
- The amount and type of bleeding
- Pain intensity and duration
- Any medications or hormonal birth control you’re using
You might also be asked to describe or show a photo of what passed, which helps in identifying whether it was a true decidual cast or another tissue type.
Tip: Bring notes or photos (if available) and a list of any medications or recent hormonal changes.
Follow-Up and Care
After diagnosis, your doctor may:
- Recommend pain management (NSAIDs like ibuprofen)
- Suggest hormone regulation therapy if imbalance is detected
- Schedule a follow-up ultrasound in 2–4 weeks
- Advise rest and hydration for recovery
If the cast formed due to hormonal contraceptives, your doctor might adjust your dosage or recommend an alternative birth control method to prevent recurrence.
FAQs
Q1: Do I need an ultrasound after a decidual cast?
Yes, in most cases your doctor will recommend an ultrasound to ensure no residual tissue remains and to rule out pregnancy-related complications.
Q2: What should I bring to my appointment?
Bring a detailed symptom log, photos (if available), your menstrual history, and a list of any medications or hormonal contraceptives you’ve been using.